Sclerotherapy is one of the most popular treatments for varicose and spider veins. If you look through the before and after shots of some of our patients, you’ll see ultrasound guided sclerotherapy and direct vision sclerotherapy features repeatedly. It’s been a reliably used treatment for 50 years. In today’s blog, we want to delve deeper into what happens when a diseased varicose vein is injected with sclerosant and why this treatment works. Let’s begin by understanding why varicose veins occur and why they need to be treated.
What are varicose veins?
In a healthy vein, blood moves in one direction thanks to one-way valves on the interior of the vein, preventing blood from moving backward. Varicose veins occur when faulty one-way valves allow blood to leak backward and collect in a section of a vein. This is known as venous insufficiency, as the vein becomes ineffective at returning blood to the heart. The pooling blood inside the vein can make the vein protrude on the surface of the skin, looking tortuous and blue. Sufferers may notice symptoms such as pain, cramping, tired or heavy legs, as well as itching, and swelling. This condition affects approximately 30% of both women and men at some point in their lives. Its cause is linked to hereditary factors but can be exacerbated by professions where standing for extended periods is necessary and the extra pressure placed on veins during pregnancy. Removing varicose veins is necessary to resolve painful symptoms and restore normal circulation. It can also help to avoid deterioration into more chronic venous disease which is a progressive condition associated with a variety of complications. Varicose veins do not heal themselves and may only worsen without treatment – medical attention is necessary. In years past, the only option was vein stripping, which meant minor surgery to cut the section of vein out. This method of treatment was painful and had a high recurrence rate. The far less-invasive treatments used today (like sclerotherapy) employ the function of sclerosis to “remove” the problem vein.
What is sclerosis? What can it do for varicose veins?
Sclerosis is a technical word which can be essentially translated to “a hardening over” of a particular part of our body, whether it be blood vessels, skin or nerves (such as in multiple sclerosis). Sclerosis can be bought on by inflammation, autoimmune conditions, trauma, and acute injury. For varicose veins, when a sclerosant is injected into a varicose vein, the sclerosant will permanently damage the internal lining of the vein wall. This will then set off an inflammatory cascade which eventually leads to the vein hardening over or becoming solid “dead” material. Once this has happened, the body will recognise this sclerosed dead vein as non-viable material and begin to absorb the vein. Break down and absorption of the sclerosed vein can take many months and will depend on the person’s immune system in general. Many modern varicose vein treatments utilise the acute injury reaction to bring on sclerosis in varicose veins:
- Thermal injury – endovenous laser ablation or radiofrequency ablation
- Biochemical Injury – direct vision sclerotherapy, ultrasound guided sclerotherapy using sclerosants
- Adhesive/Thermal Injury – use of modern-day medical grade superglue for vein treatment
- Chemical Injury – injecting powerful chemical agents into the vein (this is no longer used in practice due to the potential complications).
There are currently 2 Sclerosants in use in Australia
- Sodium Tetradecyl Sulphate (abbreviated STS) is used to treat telangiectasias, reticular veins and large varicose veins.
- Polidocanol (abbreviated POL) is used to treat large and small veins.
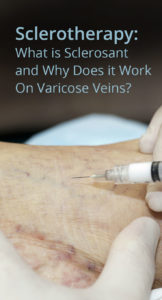
What happens during sclerotherapy treatment?
As with all varicose vein treatments at Vein Health (part of the Paras Clinic), a duplex ultrasound is performed to help map out the problem veins. This includes identifying unseen feeder varicose veins beneath the skin. If there are no underlying feeder veins, direct vision sclerotherapy will be used by the phlebologist to treat the veins on the skin surface. Where varicose veins are present that are not visible on the surface of the skin, ultrasound guided sclerotherapy may be used. In the case of incompetent saphenous veins, endovenous laser ablation may also be used in combination with sclerotherapy.
Key Takeaways
- When a sclerosant is injected into a problem vein, the substance causes an injury to the vein wall. This causes sclerosis of the vein. The vein collapses on itself, hardens and heals. Blood is automatically rerouted to other healthy blood vessels.
- Sclerotherapy is effective, non-invasive, and a relatively quick in-clinic varicose vein treatment.