What is Lipodermatosclerosis?
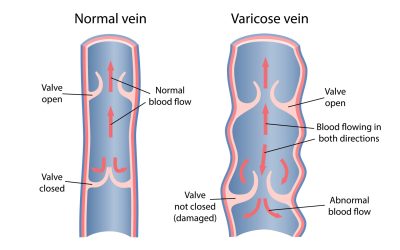
Lipodermatosclerosis is a condition that arises from chronic venous disease, primarily due to impaired blood flow in the leg veins. When veins struggle to pump blood back to the heart due to weakened or damaged valves, blood starts to pool in the lower legs, leading to a build-up of pressure within the veins—a condition called venous hypertension. This high pressure eventually causes blood plasma (the liquid component of blood) to leak out of the veins and into surrounding tissues, which worsens the problem.
How Lipodermatosclerosis Develops
The leakage of blood plasma into the tissues, combined with prolonged pressure, creates inflammation and triggers changes in the surrounding skin and soft tissue. When plasma leaks into the tissue, it brings along proteins and inflammatory cells that trigger a local immune response. Over time, these proteins settle, leading to fibrosis, or hardening of the tissue, which creates the thick, tough skin characteristic of lipodermatosclerosis. This trapped fluid also limits oxygen flow to the area, compromising the skin’s ability to repair itself.
How Lipodermatosclerosis Presents
Lipodermatosclerosis often appears as a red or brown discoloured area of skin around the lower legs and ankles, which feels hard and tender. The skin can become shiny, swollen and tight, sometimes taking on an inverted “champagne bottle” shape, with narrowing above the ankle and swelling in the calf. The area may be painful, warm to the touch, and cause discomfort when walking or standing, limiting mobility and daily activities.
Effect on the Patient and Long-Term Consequences
For patients, lipodermatosclerosis can be both painful and limiting. The affected skin and tissue become more prone to damage and may struggle to heal due to decreased oxygen and nutrient flow.
Left untreated, lipodermatosclerosis can lead to serious complications. The hardened skin and tissue make it easier for ulcers to form, especially around the ankles, as the skin’s elasticity and resilience are compromised. These venous leg ulcers are not only painful but can also be difficult to heal, and prone to infection. Additionally, lipodermatosclerosis can further aggravate chronic venous insufficiency, increasing pressure within the leg veins and intensifying the cycle of tissue damage and inflammation.
When lipodermatosclerosis reaches this stage, medical intervention, such as Sclerotherapy or Endovenous Laser Ablation (EVLA), is typically recommended. These procedures target the underlying venous insufficiency, helping to reduce pressure and prevent further plasma leakage, offering the best chance for healing and reducing any complications.
Key Takeaways:
- Root Cause: Caused by chronic venous insufficiency, leading to high pressure in leg veins.
- Plasma Leakage: Vein pressure causes plasma to leak into tissues, worsening inflammation and hardening.
- Visible Signs: Discoloured, swollen, and painful skin around the lower legs and ankles, often with an “inverted champagne-bottle” shape.
- Health Impact: Can lead to painful, hard-to-heal ulcers without treatment.
- Effective Treatment: Advanced cases benefit from sclerotherapy or Endovenous Laser Ablation (EVLA) to target the underlying vein issues and prevent complications.