Everyone is unique. Varicose veins can affect people in several ways and one person’s journey may be different to another’s. If you are an active person, you may experience symptoms of varicose veins differently to someone who is say, in a sedentary job where they’re continually sitting. Or perhaps if you have experienced pregnancy, you may have symptoms show up differently to someone who hasn’t.
Today let’s discuss a recent patient treated by Dr Paraskevas to help us understand more about how the symptoms of varicose veins are sometimes experienced and the process of getting treatment.
Janelle* is a 40-year-old woman in generally good health. She has three young children and a history of varicose veins. After her second and third pregnancies, the vein symptoms worsened. Her legs would feel heavy and uncomfortable. When she had been standing for long periods or after exercising, her legs would swell up.
What are the symptoms of varicose veins?
Varicose veins can range from small spider veins to quite large, protruding veins in the legs and groin region. The range of symptoms can vary from person to person, but in general, when we speak about the symptoms of varicose veins, here is how they are commonly felt:
- aching and pain in the legs
- a feeling of heaviness or fatigue in the legs
- throbbing
- itching legs or a burning sensation
- cramps and restless legs (especially at night)
Other things to note: as well as the legs, they can also occur in the groin and pelvic region and can occur in both men and women.
Are varicose veins always visible?
No. Varicose veins can be present even when you cannot see them. That sounds a bit like they might be lurking inside every leg – but in fact, it’s more that diseased veins don’t always appear on the surface, they can be deeper inside the leg. Patients who have varicose veins occur deeper inside the leg will have the same kind of symptoms discussed above, but they may not have any visual signs on the surface of the skin. So, if you are experiencing these kinds of symptoms and don’t know why, it may be that varicose veins are what’s causing you this discomfort.
A consultation with a phlebologist
After taking a medical history with patients, the phlebologist will perform a thorough physical examination followed by a detailed ultrasound (performed either by the phlebologist or vascular sonographer). This tells the doctor all they need to know about your condition, and based on these examinations, they can decide the best course of action for treating a vein condition.
What is CEAP?
Part of diagnosis of a vein condition is a patient’s CEAP classification. This is a way for phlebologists and health professionals to define the severity of vein disorders. This acronym stands for Clinical Etiology Anatomy Pathophysiology. Clinical – What does the patient’s vein look like? Etiology – Is the problem inherited or some other cause? Anatomy – Which veins are involved? Pathophysiology – Which direction is the blood flowing (normal or abnormal), and is blood flow blocked?
These are the classification levels:
CEAP 0 – No visible or palpable signs of venous disease
CEAP 1 – Superficial spider veins, telangiectases, or reticular veins
CEAP 2 – Varicose veins only
CEAP 3 – Ankle oedema (swelling) of venous origin, not foot oedema
CEAP 4a – Dermatitis/eczema and/or hyperpigmentation
CEAP 4b – Lipodermatosclerosis and or atrophie Blanche
CEAP 4c – Corona phlebectatica paraplantaris (CPP)
CEAP 5 – Healed venous ulcer
CEAP 6 – Active venous ulcer (open sore)
In Janelle’s case, her CEAP classification is CEAP 2, 3 – that is, she has varicose veins with swelling (oedema) in the tissues of the peripheral vascular system.
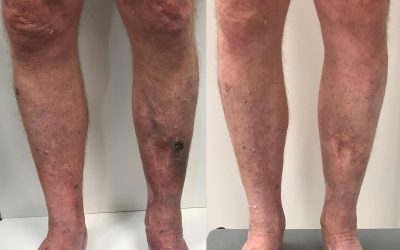
Before and after, left inner leg

Before and after, right inner thigh
What is the great saphenous vein?
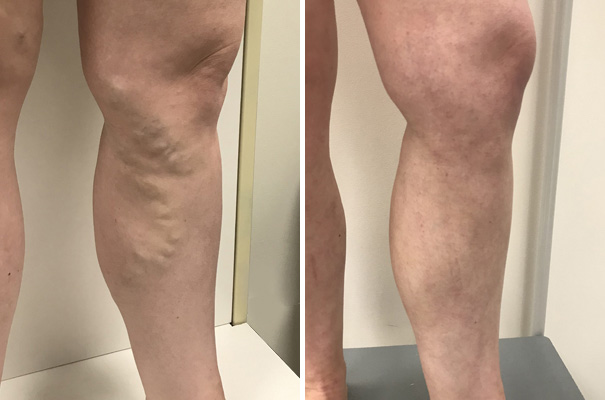
Janelle’s physical and ultrasound examination revealed that the underlying great saphenous veins were incompetent (leaking backward) in both legs. The great/long saphenous vein is the longest vein in the body. It runs along the length of the legs from the front of the ankle, up into the groin where it joins the main vein (common femoral vein). Blood is diverted from the great saphenous vein into the deep veins and from there, blood can then return to the heart. However, if the great saphenous vein is incompetent, it is unable to perform this function. Blood will pool within it and then push into the surface veins of the leg and ankle with gravity, where it can cause discomfort, heaviness, tiredness, even swelling, and skin changes, including ulceration. The visible varicose veins you can see in the images of Janelle’s legs before treatment were directly related to a “leaky” or incompetent great saphenous vein that was not able to divert blood into the deep veins efficiently. Over time, blood was pushed into the surface branches.

Before and after
Janelle’s treatment schedule
The treatment Dr Paraskevas undertook for Janelle involved Endovenous Laser Ablation of the great saphenous veins (under local anaesthetic and performed on both legs on the same day) and follow up Ambulatory Phlebectomy and Ultrasound Guided Foam Sclerotherapy (again provided under local anaesthesia and with regional nerve blocks).
Janelle was able to continue with her normal activities of daily living during her treatment schedule, which predominantly involved looking after her 3 children.
Follow up of her progress has occurred over the last 12 months and photos were taken today of her legs exactly 14 months since her Endovenous Laser Ablation procedure. Dr Paraskevas also conducted a follow-up ultrasound. This shows no residual or recurrent veins and her symptoms have completely disappeared. We will keep monitoring her progress over the next 5 years to ensure a good long-term outcome.
*The patient’s name is been changed to preserve her privacy.
Key takeaways
- Not everyone will experience the same symptoms of varicose veins, but they may experience some of the following: aching, pain, heaviness or fatigue, throbbing, itching, a burning sensation, cramps, and restless legs.
- There is a period of time when the treated veins will be tender, inflamed and the legs are recovering from the treatments. Patients are always advised to be patient as the healing phase can take up to 12 months and sometimes, longer.
- The CEAP classification allows phlebologists and health professionals to categorise the severity of vein disease.
- These are the treatments Janelle received for her varicose veins Endovenous Laser Ablation, Ambulatory Phlebectomy, and Ultrasound Guided Foam Sclerotherapy