Varicose veins are often dismissed as a cosmetic problem. These ropey, blue blood vessels that protrude from the surface of the skin cause some people to shy away from baring their legs in shorts or dresses. But are they dangerous? Many think this is just a question of leg aesthetics if they’re concerned about a varicose vein, but perhaps those people have not suffered from the painful symptoms that come along with the prominent veins. This can be a progressive condition, with increasing severity as time passes.
It’s true that varicose veins can be a challenge to self-esteem and cause a loss of confidence, which in itself is reason enough to do something about them should you want to, but they typically cause painful symptoms that can be debilitating. Varicose veins are a genuine health concern.
What are Varicose Veins?
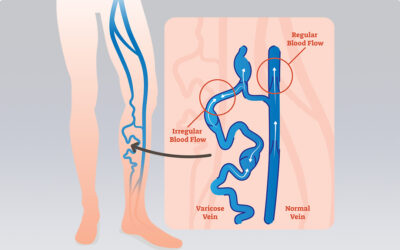
Varicose veins are leg veins that no longer function correctly. These veins fail at their purpose: to return blood from the extremities to the heart and lungs. One-way valves line the interior walls of our veins, which causes blood to flow in one direction only. However, due to factors such as genetics, hormonal fluctuations, being constantly on your feet, etc – the one-way valves fail, allowing blood to leak backward and not to be effectively driven forward (venous reflux). The blood pools, the diameter of the vein is stretched, and this pressure build-up is why you see bulging veins on the skin’s surface.
While incompetent veins are often found in the legs, they are also commonly found in the pelvic region.
Causes of Varicose Veins
The definitive cause of varicose veins is not known, but a family history of the condition is a strong indicator that you may get them too. Up to 30% of women and men are affected by varicose veins. Women may experience them earlier in life than men, with fluctuations of hormones, such as during puberty, pregnancy, menopause, and with the use of birth control pills.
What are the health consequences of not having varicose veins treated?
As soon as you establish that you have varicose veins you should see a phlebologist. As time goes on, varicose veins may deteriorate and lead to serious complications such as severe skin changes (pigmentation, eczema, and lipodermatosclerosis) or open sores (venous ulcers). Some of these complications can cause permanent damage to the lower legs and ankles and can be difficult to treat when they are severe. Varicose Veins also increase your chances of developing blood clots, which is considered an extremely severe condition.
Here are the symptoms and complications of varicose veins as they progress:
- swelling or puffiness in the leg (oedema)
- venous eczema (venous dermatitis, stasis dermatitis)
- discolouration of the skin (hyperpigmentation)
- thickening of the skin of the lower leg or ankle (lipodermatosclerosis)
- localised or extensive breakdown of the skin creating open sores, often around the ankle region (venous ulcer or leg ulcer)
Lipodermatosclerosis, where the skin thickens can affect the health of the lower leg and lead to complications such as severe inflammation (phlebitis) and infection (cellulitis). Blood clots can form (thrombophlebitis) when the body confuses the pooling of blood in the vein for bleeding. The body sends cells to stop the bleeding, which creates the clot. This obstructs blood flow, and if/when it breaks off, it can be life-threatening, depending on whether it is a deep vein or a superficial vein and its capacity to move to the major organs.
These symptoms can often be observed in older people who have had varicose veins for a long time and not sought treatment. But people in their 30s, 40s, and 50s can also experience some of these symptoms of severe varicose veins, along with painful throbbing, swelling, and heaviness which can impede mobility and a restful night’s sleep.
Varicose vein treatment
Today’s treatments for varicose veins don’t require a lengthy hospital stay, most varicose veins can be treated on an outpatient basis. Procedures available for varicose veins include:
VenaSeal
This method entails the use of a special glue to treat diseased veins by sealing the affected vein closed. VenaSeal glue is a medically approved adhesive that seals the saphenous veins at the thigh. The sealing causes the vein to harden and is eventually absorbed into the body.
Endovenous Laser Ablation
A laser fibre is inserted into the affected vein through a small incision, then the fibre is slowly removed. The vein wall collapses with little discomfort. This method is one of our most frequently used treatments and replaces stripping varicose vein surgery, which was a common and invasive procedure of the past.
Ultrasound Guided Sclerotherapy
In this treatment, an ultrasound examination is carried out on the affected leg to map out the problem veins. This includes diseased veins not visible to the naked eye. A sclerosant solution is injected into the problem veins causing the vein wall to collapse, heal, and finally be absorbed into the body.
Varicose veins are more than just a cosmetic problem, they are a sign that you need treatment to avoid painful progression of symptoms. Your phlebologist may use one or more of these treatment techniques to treat your varicose veins, deciding which to use based on the diameter and location of the blood vessels, and the severity of your condition.
Key Takeaways
- Varicose veins are veins that are no longer functioning correctly (they are not efficiently returning blood to the heart).
- Untreated varicose veins may progress into chronic venous disease whose symptoms include swelling, venous eczema, hyperpigmentation, thickening of the skin, open sores, severe inflammation, cellulitis, and blood clots.
- Treatments available include VenaSeal vein glue, endovenous laser ablation, and ultrasound guided sclerotherapy.